Your Next Team-Building Project: Make the Appeal or Take the Penalty!
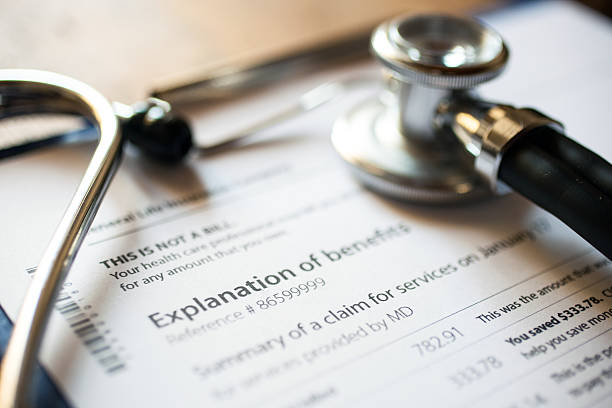
Healthcare facilities have to get their game-face on as their bottom lines are taking some personal fouls and penalties. One out of every ten health care patient claims will be denied at a cost of nearly 2% of net patient revenue each year. (Brand, R & Fontana, E, 2019) How hard does your Revenue Cycle staff work to process those 10 charts as a futile effort? This is not cost-effective.

This is not just an inpatient or outpatient problem nor is it a sporadic anomaly. In 2011, $3.9 million dollars was written off (1.1%NPR). In 2017, the losses increased to $7.4 m. million dollars (2.1% NPR). This is a 90% increase in write-offs for the average 350-bed hospital between 2011 and 2017. There are three (3) main causes for the increase in denials.
- An increase in automated data reviews by government entities & insurance carriers
- Increasingly complicated criteria
- The “fine print” in facility/carrier contracts
Automated computer-generated reviews identify DRG downgrades and scan for medical necessity issues with lightning speed and deny payment. Health Insurance carriers and the Centers for Medicare and Medicaid Services (CMS) are creating highly complex requirements for a claim payout. The “fine print” included within the facility-insurance carrier contracts is requiring a closer look at technical specifications and meeting the requirements for “medical necessity” criteria. (Brand, R & Fontana, E, 2019)
The Centers for Medicare and Medicaid Services (CMS) further reduces the amount of facility reimbursement through Recovery Audit Contractors (RAC). RAC reviewers help identify program vulnerabilities and advise them on what corrective action to take to reduce improper payments. In the last three-year repayment RAC review, $192.8 million dollars was prevented due to improper payment codes (pre-payment). That figure is less than .3% of the number of claims submitted each year. In addition to RAC reviewers, the CMS also created a Recovery Audit Contractor Data Warehouse. This is a tool for measuring the performance of RAC reviewers and to prevent duplicate reviews of the same claim. This warehouse can also be accessed by facility compliance officers to review areas where the complicated criteria can be further explained. (CMS, 2010)
In addition to payments being denied, there are also financial losses due to improper payments; charges that are being paid for a reduced amount for reasons including
- Lack of documentation supporting the ordered service or treatment
- Services billed do not meet the CMS’ medically necessary criteria
- Services are incorrectly coded
(CMS, 2015)
So who can act as the referee through this process? What are the options to prevent CMS/Insurance denials, underpayments for rendered services and treatments, and who will make appeals on your behalf? How can we reduce the number of appeals needed for RAC reviews OR how can we reduce the number of potential RAC reviews in the first place?
With all of these questions, let’s call a timeout to review a great game plan:
- Know your facility’s most common DRGs
- Focus on medical necessity and patient status as they are the highest denial areas
- Focus on the “Patient Financial Experience”
- Build relationships with your Payer representatives
When the focus is turned inward, there is a better understanding of who plays what role and has what responsibility within the Revenue Cycle. A facility should regularly review their most common Diagnosis-Related Groups (DRGs) and what the highest denial codes are and put their primary focus in those areas. The “Patient Financial Experience” can best be described as the journey from scheduling the appointment or procedure to the closing of the patient’s account. The goal is to provide consistent quality-focused interaction where each team member is remembered as “providing excellent service and care.” Research has found that allowing the payer to review medical records for up to 48 hours after admission in exchange for presumptive authorization of patient status for same-day and ED admissions reduced denials by 100% (in these specific areas). It can be a win-win for both the payer and the Revenue Cycle team. The payer reduces the amount of denial documentation and the Revenue Cycle team knows what information that payer needs to approve the medical care and treatment on the first submission in addition to receiving the full payment amount for the services rendered. (Brand, Robin, August 2018)
The best defense is to have a great offense! Today’s healthcare facilities are being scrutinized as never before and are being forced to do more work with fewer people. Consider bringing in an Appeal(s) Management/Recovery Team. Appeal(s) Management Service Providers have a professional team (often including RAC auditors) with unique skill-sets that can reduce denials and audits, lower the cost of appeals, and improve documentation and coding accuracy. This group of specialists can perform an external review of medically necessary past and present discharges with a focus on one-day stays and observation status codes in addition to the most common DRGs. This step identifies the patient status issues and medical necessity diagnosis codes that may need further investigation or additional education for the coding team. The review also looks at past denials, current appeals and the dollar amount associated with them.
Some questions to ask the company could include whether they also work to develop payer-facility working relationships that enable both sides to reduce claim denials in the first place? Do they constantly review the CMS website, the OIG and RAC web postings for new updates as well?
In the Revenue Cycle process, everyone has their own level of expertise. Make sure the Appeal(s) Management service provider you choose complements your facility’s staff.
It is important to look at the Appeal(s) Process as a Team-Building activity. It brings all the key players together to take a magnified look into the claims submission steps in addition to the process of assigning the proper codes that reflect the patient’s Electronic Health Record (EHR). Bringing in some help for the Offense ensures you have the best game plan when it comes to denials, audits, and appeals.
When you are ready to build your dream team, consider IdeaCentre HIM Solutions as your “star player” to build the best offense for your facility. Remember, the BEST defense is a GREAT offense.
References:
Brand, Robin, August 2018, Questions and Answers found on January 2020 from https://www.advisory.com/research/revenue-cycle-advancement-center/at-the-margins/2018/08/sharp-healthcare
Brand, R & Fontana, E, March 2019, Why Your Denials are Skyrocketing found on January 10, 2020 from https://www.modernhealthcare.com/revenue-cycle/why-your-denials-are-skyrocketing-and-3-ways-hospitals-can-respond
CMS, 2010, Implementation of Recovery Auditing found on 1/13/20 from https://library.ahima.org/PdfView?oid=105077
CMS, 2015, Recovery Auditing in Medicare Fee-For-Service found on 1/8/20 from https://www.cms.gov/Research-Statistics-Data-and-Systems/Monitoring-Programs/Medicare-FFS-Compliance-Programs/Recovery-Audit-Program/Downloads/FY2015-Medicare-FFS-RAC-Report-to-Congress.pdf
Recommended Posts
The Secrets of Building an Unsinkable Business
February 27, 2023
Next Level Audits
May 12, 2022

IDEACENTRE: THOUGHT LEADERS IN THE HIM INDUSTRY
March 13, 2021
